What is the Collaborative Care Model?
The Benefits of Collaborative Care
What Are the Fundamentals of a Successful Collaborative Care Model?
Building A Proper Team for Mental Health Collaboration
Key Tools and Technologies for Providers to Use
Telehealth
Billing and RCM Software
Practice Marketing
Healthcare Dashboards
Speak with one of our Healthcare Experts today.
Collaborative care models are in the healthcare spotlight these days. Although the terms collaborative care and integrated care can vary in meaning, they are often used interchangeably. The purpose of this model of care is to bring behavioral health and primary care providers (PCPs) together to provide patients with whole-person care, thus improving healthcare delivery.
As integrated care models gain popularity, care managers, patients, and providers alike still have questions about how they work. Not only is it important to understand the various meanings of the different terms for collaborative and integrated care, but it is also helpful to be aware of the many benefits of this care model, as well as the steps and technologies needed for its proper implementation. Read on to find the answers to these questions and more.
What is the Collaborative Care Model?
When addressing the topic of the “collaborative care model,” it helps to take a step back and consider the different meanings this term has. Collaborative care refers to a spectrum of care models – or think of it as a broader term encompassing types of care models with more specific meanings. Among these are coordinated care, co-located care, integrated care, and more.
Generally, all collaborative care models aim to help care managers improve the organization and management of patient care, as well as the outcomes of patient care. This is accomplished by bringing together both a patient’s primary care provider (PCP) and behavioral health provider to determine the best care for a patient.
The level of cooperation between these two entities varies at times. Different collaborative care models exist for levels of cooperation such as:
- Coordinated care generally refers to a care model that involves some coordination and information sharing between providers with each practice maintaining largely separate administrative units.
- Co-located care generally refers to a care model in which a patient’s primary care and behavioral health providers are in the same physical location but are effectively separate administrative units.
- Integrated care generally refers to a care model where a patient’s medical care and behavioral health care are both owned and operated by the same practice allowing the patient to receive whole-person care in one plan, and often in one location. “Integrated care” is synonymous with collaborative care as a whole.
While the above types of collaborative care models are not the only ones in existence and vary widely, the overall takeaway is that these models help patients achieve better outcomes with reduced costs. By eliminating barriers between providers, care managers can do a better job of helping a patient get the care they need as a whole person while meeting the patient’s special health requirements.
Other terms to be aware of that are related to collaborative care include “whole person care” or “no wrong door.” Whole person care refers to a holistic style of care that encompasses all patient needs. No wrong door refers to the concept that patients should be able to seek for mental health care or physical health care at any of the available providers so that there is “no wrong door” to enter when choosing a provider for their various health needs – so that patients get the care they need, where they need it, and when they need it.
Regardless of a patient’s physical health conditions or mental health conditions, it’s important for them to have easy access to care. Bringing together health professionals and mental health specialists to develop a treatment plan for patients with mental disorders or substance use issues can help increase clinical outcomes across the industry as a whole.
The Benefits of the Collaborative Care model
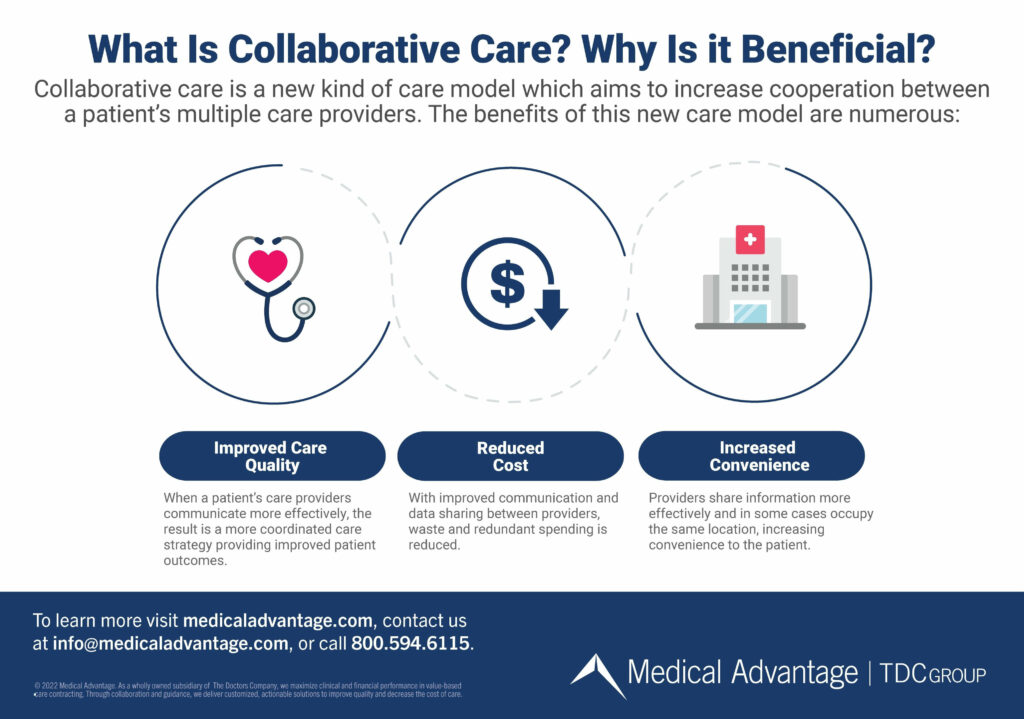
Now that the definitions of the collaborative care model have been established, we will go deeper into each of its benefits.
Improved care quality. The collaborative care model is beneficial to patients on many fronts. However, the most powerful of these is the simple fact that the collaborative care model is known to improve care quality.
When primary care and behavioral health providers communicate more effectively with one another, the result is a more coordinated and effective care strategy that improves patient outcomes. Or in the case of some integrated care models, these providers are one in the same provider.
Reduced cost. Another benefit of integrated care models not to be overlooked is cost savings. One of the largest contributors to healthcare costs is wasteful spending from redundancy and integrated care models help to combat this. Enhanced communication and data sharing between a patient’s care providers reduces the need to perform tests and procedures multiple times.
Collaborative care serves in this way to cut costs by providing a powerful form of preventative care. As the old saying goes, an ounce of prevention is worth a pound of cure. Nowhere is this truer than in collaborative, whole-person care. By addressing all a patient’s needs – both physical and mental health care – providers not only see better outcomes, but reduced costs as well.
Increased convenience. Collaborative care – particularly with co-located and integrated care models – also has the benefit of saving time and increasing convenience to both patient and provider.
With both primary care and mental health services located on one site – or committed to an increased level of communication, at minimum – the amount of time needed for referrals, transportation, and retrieving records from one another will be reduced.
Return on investment. Implementing an entirely new care model is no small task for healthcare providers who, justifiably, may have reservations about changing their business model. But the upside is that integrated care models can lead to large returns on investment.
As the American Psychiatric Association (APA) mentions, collaborative care is shown to help cut costs and reduce waste. As this cost reduction continues due to the aforementioned reasons of reducing waste spending and redundancy, many are shocked to learn that they can also increase revenue. With the current emphasis on value-based care – where payers reimburse more for higher quality care – improving patient outcomes is key for increased revenue, and the collaborative care model does exactly that.
What Are the Fundamentals of a Successful Collaborative Care Model?
While the specifics of each integrated care model vary, nearly all successful collaborative care models tend to incorporate the following elements:
Effective data-sharing. Effective data and records sharing impacts each setting, whether the primary care and mental health providers joined via a collaborative care model, are one in the same practice, operate under the same roof, or simply participate in the model together. Sharing patient registry data is key when a primary care physician is working with a consulting psychiatrist.
Streamlined referrals. In integrated care models, the process of referring patients from the primary care setting to a psychiatrist or other mental health specialists – or even the other way around – must be as seamless as possible. In the case of referrals, the more closely aligned the two practices are the more effective they will be – collaborative care good, co-located care better, and integrated care best.
Integrated scheduling. An overarching concept behind collaborative care is that the agendas between a patient’s care providers should be more unified. This holds true in terms of scheduling. A successful collaborative care approach will require all the providers involved in a patient’s care providers to cooperate and coordinate scheduling so that conflicting agendas are avoided.
Prioritize co-location. It is no secret that change can be frustrating, disruptive, and costly for medical practices. Adopting collaborative care models (like choosing to co-locate or even merge primary care and mental health providers) can be complicated and costly up front, but the benefits are huge in the long term.
While these roles and responsibilities can vary, getting the most out of your collaborative care model requires buy-in from everyone involved. This includes your patient, primary care provider and behavioral health provider, specialists, and care manager who helps to connect and oversee the entire network.

Building A Proper Team for Mental Health Collaboration
Efficient team structure is of the utmost importance for integrated care models. With so many different individuals and entities working together to provide a patient with effective care, the proper setup of roles and responsibilities is key to presenting a coordinated front.
Of course, a successful team is as much about personnel as it is about policies. Creating effective workflows is key to helping facilitate the flow of information and the delivery of quality care within the collaborative care network.
Key Tools and Technologies for Providers to Use
Effective workflows encompass EHR (Electronic Health Record) and documentation, scheduling, effective referrals, and especially care management. Further, the components of collaborative care models are telehealth, billing, and RCM (Revenue Cycle Management) software, practice marketing, and healthcare dashboards.
Telehealth
Thanks in part to a surge in both telehealth usage and the demand for mental health services during the COVID-19 pandemic, virtual visits and mental health have become increasingly associated with one another as it helps patients feel more comfortable amidst the stigma surrounding mental health. This means practices that seek to provide mental health services, like those within collaborative care models, would do well to embrace telehealth software if they have not already.
Billing and RCM Software
Collaborative care models can dramatically impact a practice’s ability to be effectively reimbursed for care due to increased cooperation between mental health and primary care providers. Records, visit documentation, and other forms of data required for reimbursement by payers are then more organized and centrally located. This makes the necessary data easier to find and submit when billing and revenue cycle management workflows come into play.
Practice Marketing
Adopting an innovative new care delivery method (like the collaborative care model) is a smart move, but patients need to be made aware of the benefits of this model and encouraged to utilize it. Enter practice marketing, a host of services used to help practices grow and maintain their patient base by educating patients about the benefits of the collaborative care model.
These services include website setup and maintenance, online reputation management, social media outreach, pay-per-click online advertising, and more. In addition, a strong and positive online presence can help your medical practice attract and recruit talent, as well.
Healthcare Dashboards
It is no easy task to bring together the myriad reports, databases, and records systems from both mental health and primary care practice. Fortunately, software known as healthcare dashboards exists. This software helps healthcare groups consolidate a wide variety of clinical, operational, and financial data into one easy-to-use and automatically updated software “dashboard.”
Dashboards help improve medical care efficiency, benchmark key performance indicators, and more. They are a powerful resource for care managers seeking to gain an overview of the many data present for patients in collaborative care models.
Medical Advantage Can Help
Collaborative care models, or integrated care models, unveiled an exciting new frontier in healthcare. Here, we can expect to see improved outcomes, reduced costs, and increased revenue by facilitating cooperation between behavioral health and primary care providers.
However, these changes can be intimidating, as pivoting to a new care model is not without its challenges. Medical Advantage supports this process at every stage. Our experienced consultants hail from healthcare, IT, behavioral health, and coding backgrounds. Our team works virtually, and at the point of care to help organizations of all sizes implement collaborative care models. To find out more, contact one of our consultants today.






