Value-based care programs rely on financial risk adjustment to reward providers who successfully care for complex, high-risk patients. Risk adjustment is a statistical method used to offset the cost of providing healthcare to individuals, especially those suffering from chronic conditions, who pose a high risk to insurers.
The financial reward from these programs heavily depends on how completely providers report diagnosis information on their claims, since these diagnoses are used to assess financial risk. High-risk patients whose conditions are not completely reported will appear healthier and less risky than they are, therefore, the payer will pay the provider less, even if excellent care is provided.
Accurate risk measurement depends on several steps. A failure at any step may lead to underreporting and undermeasuring risk, meaning poorer physician performance in value-based care programs.
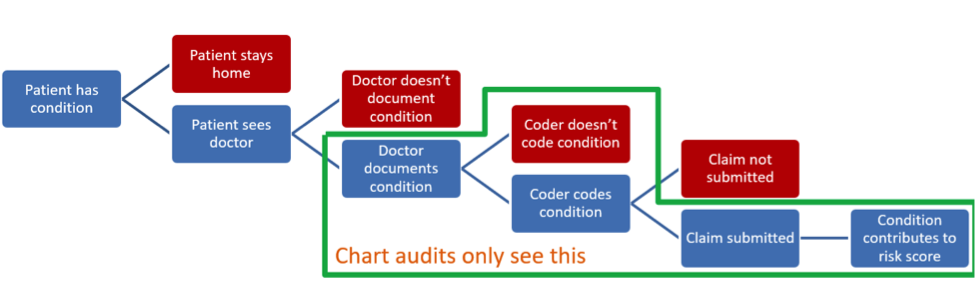
FIGURE 1. NECESSARY STEPS FOR PATIENTS’ CONDITIONS TO CONTRIBUTE TO RISK ADJUSTMENT
Risk measurement is broader than translating documentation into diagnosis codes, which is what audits typically assess. If a patient needs care but stays home instead of visiting the physician, diagnosing the patient’s condition can be delayed or missed entirely, perhaps manifesting later as an expensive hospital visit. Likewise, a physician may be aware of a diagnosis but fail to document it, meaning that the coder does not record it. If care is performed but not billed, the practice absorbs the cost of the care and misses the opportunity to report diagnoses on the unbilled claim, leading to further decreased payment through value-based care programs.
Tips to improve risk reporting and patient care:
1. Proactively schedule visits with all patients
Scheduling visits with patients well in advance and reminding patients of upcoming visits can reduce missed visits and ensures patients with chronic conditions receive appropriate care. This also encourages patient engagement with the practice and reduces emergency department visits.
2. Preventive care visits are excellent opportunities to document conditions
Office visits for preventive care and care planning, particularly in primary care but also for specialists, help patients manage their conditions and ensure they’re adhering to their medications. At the same time, the provider can completely document and code the patient’s conditions. The Center for Medicare and Medicaid Services’ (CMS) recommends that annual wellness visits are an excellent opportunity to do this for Medicare and Medicare Advantage patients.
3. Keep staff communication lines open
Frequent and open communication between clinicians, coders, and billers can help clinicians clearly document patients’ conditions, while also helping coders record diagnoses more completely and specifically. Formal and regularly updated training of coders and billers also helps improve documentation. Complete and reliable medical records facilitate patient care, particularly since health records are increasingly shared between providers.
Learn more about Medical Advantage’s work to improve risk reporting while improving quality and outcomes for patients in our white paper below.





