As leaders in the geriatric care field work to solve today’s problems, they see what is on the horizon for the demographic they serve. Forbes reports that the 65+ population in the United States is expected to double from about 50 million to 100 million by 2060. The American Hospital Association tells us that 80% of elderly patients present one chronic disease, and 77% of these patients will develop at least two. This has given rise to the concept of age friendly health systems.
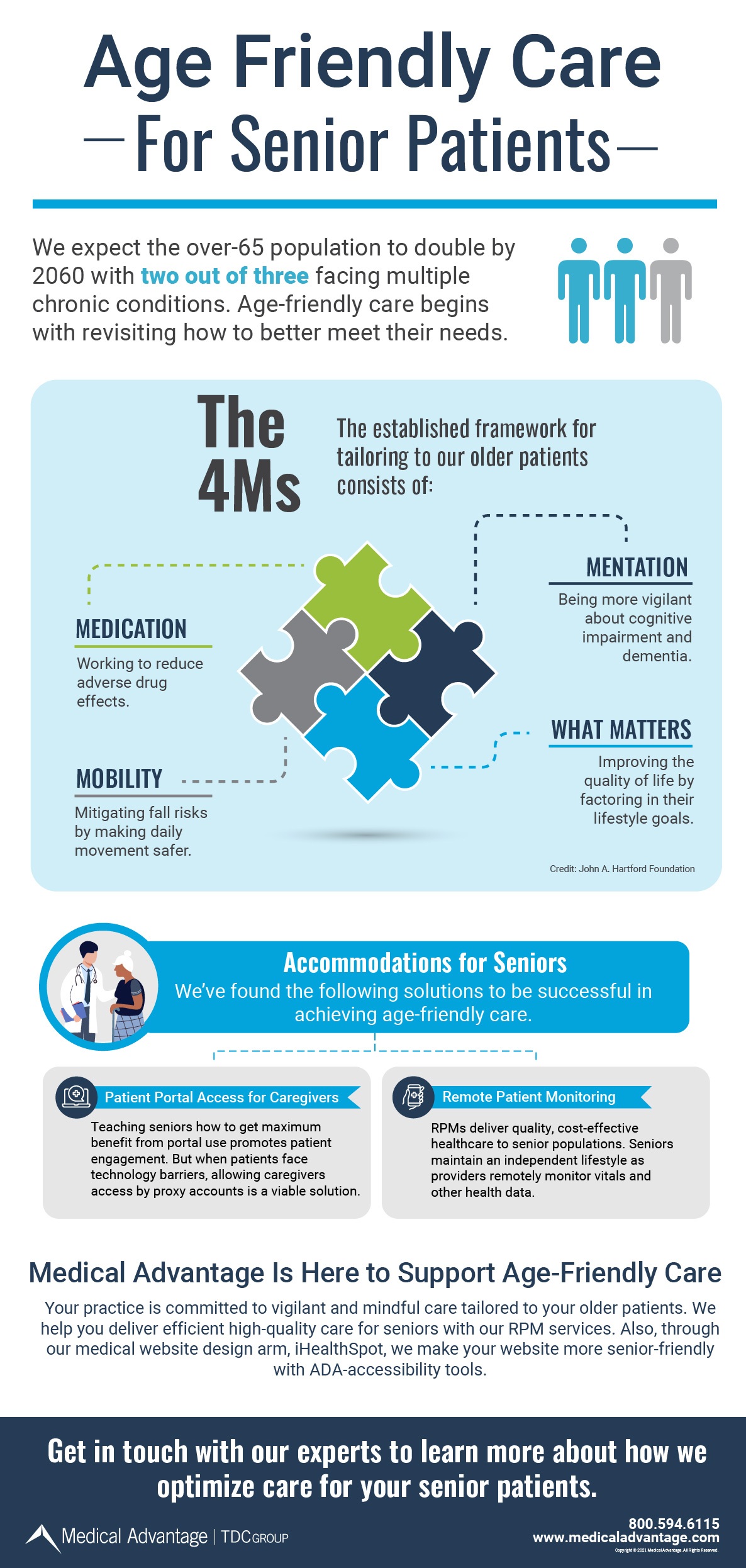
In partnership with the Catholic Health Association of the United States, The John A. Hartford Foundation initiated the Age-Friendly Health Systems movement that is set on having 20% of hospitals adopt the 4Ms model by 2020 (a model focused on What Matters, Medication, Mentation, and Mobility). This mission is focused on sweeping change for elderly care while providing a framework built around the patient’s quality of life. Perhaps your medical practice will be the next to realize the benefits of this program.
The Current State of Healthcare for the Elderly
Among the greatest challenges of the over-65 population are frequent hospitalizations, a lack of family support, and too many medications (that are often unaffordable) joined with health problems that snowball due to inadequate intervention. Other influential factors affecting senior health are technology gaps in an internet-reliant society, barriers to transportation, financial constraints of fixed income, insufficient time to address all healthcare needs, and undiagnosed mental issues.
On the practice side, physicians are experiencing staff shortages, insufficient revenue, and not enough time to address the care of elderly patients holistically. Typically, they can only address major complaints meanwhile neglected peripheral health problems have costly consequences down the line. With understaffing comes the risk of delayed or missed lab orders, unfulfilled referrals, and a lack of critical follow-ups.
Current practices and trends in care for elderly patients are:
- Shift to value-based care and reimbursement.
- RPM (remote patient monitoring) rollout.
- CMS (Medicare/Medicaid) raising quality score thresholds.
- Mitigating hospital readmissions.
- Push for Medicare Advantage over straight Medicare.
Age-Friendly Care and the 4Ms Model as a Solution
The Age-Friendly Care movement resolutely acknowledges that the current system is harming our seniors and has gotten out of hand. As of August 2020, there are 804 Age-Friendly Health Systems recognized participants nationwide including hospitals, medical practices, retail pharmacy clinics, and long-term care facilities.
This approach is all about shifting more attention to the needs and well-being of older patients. While the financial relief of reduced hospitalizations is a value-based care benefit of an age-friendly system, there is mutual reward as the patient enjoys better quality of life in their remaining years. What’s more, this approach has much potential to stimulate patient engagement.
The John A. Hartford Foundation shared these Age-Friendly Health Systems success metrics:
- Baystate Health saw a 40% increase in meaningful changes to care plans by simply asking their elderly patients, “What matters to you?”
- Stanford Health Care reduced delirium incidents by 29% with mortality cut by 48%.
- After 4Ms implementation, Anne Arundel Medical Center reduced facility readmissions, LOS (length of stay), and ED time by a total of 10.2 years!
- CVS Health adopted the Age-Friendly Health System and the 4Ms model for older adult visits for its 1,100 Minute Clinic locations nationwide.
The AHA podcast notes how Ascension used the Age-Friendly Health System for over 10,000 annual wellness visits and saw improvements for patients in all quality measures such as the frequency of ulcers and accidental falls. Also of note, the 4M’s structure can be added to your EHR system.
What Are the 4Ms of Age-Friendly Care?
Age-friendly care structure implements four core pillars: What Matters, Medication, Mentation, and Mobility.
- What Matters – It is crucial to understand each patient’s health goals and care preferences across settings so that you provide aligned care, including their end-of-life care.
- What this might look like: “Hello. We’re giving you a quick call to check in with you. We understand that COVID-19 lockdowns have made it hard to see loved ones. We’re here to support you. How are you faring with all this? Tell me what matters to you at this time.”
- Medication – When medications are necessary, administer those with a low risk of interfering with What Matters, Mentation, or Mobility (example: some medications cause detrimental delirium for older people).
- What this might look like: “It’s been a while since we went over your current medications. Since you have them all with you, would you please pick up one pill bottle at a time?”
- Mentation – Taking the Medication principle a step further, Mentation works to prevent, identify, treat, and manage dementia, depression, and delirium among all care settings.
- What this might look like: “These times are stressful and too much stress can impact your memory, especially short-term. Are you experiencing this? I’ll also ask you some questions about the thoughts and feelings you’ve had lately.”
- Mobility – Measures taken so that older adults move about safely in their daily lives to keep functioning and do What Matters to them.
- What this might look like: “Are you able to move around the house okay?Let’s do this: Stand up and sit down in the chair without using your hands or arms to help you back up. Try to do this five times in a row.”
Other Proactive Approaches to Aging Population Healthcare Challenges
The Age-Friendly Health Systems initiative spurred a much-needed conversation about how to better serve geriatric patients. As the healthcare community moves forward with this approach, care professionals will continue to uncover more solutions to the problems both patients and medical organizations face.
These strategic measures for an improved elderly patient care landscape are currently in effect:
Appointed care managers: Providers who serve patients over 65 will benefit greatly from having a skilled Care Manager. This role ensures that elderly patients do not fall through the cracks. Consistent follow-ups and care plan tracking go a long way toward preventing health decline and decreasing hospitalization risks.
Patient education: Helping patients fully understand their medical issues and the importance of each facet of their care plan encourages patient engagement that leads to better healthcare outcomes.
Advanced care conversation: It is not easy to bring up this subject, but laying out an advanced-care plan in the here-and-now is undoubtedly in the patient’s best interest. This puts these decisions in the best hands – doctors who know the patient well, family members or caregivers, and the patient advocating for themselves.
Portal access for caregivers: The patient portal continues to be a force for patient engagement, but due to technology gaps among seniors (and some forgetfulness), older patients end up missing out on portal benefits. The remedy to this is providing a caregiver or an appointed family member access to the patient’s portal. Practices who have done so have seen success.
RPMs: Enables observations that are crucial for timely medical intervention and collects vitals and other health metrics in real-time. Meanwhile, seniors enjoy going about their lives without frequent office visits.
ACOs: When a practice joins an Accountable Care Organization network this will improve patient care quality. By collaborating with an ACO, geriatric care medical practices can better identify patient needs, connect patients with needed community resources, detect quality gaps, and keep up with CMS requirements and changes. “Being a part of a physician organization, such as an ACO, helps physicians improve the quality of care they are providing their patients and the quality of life their patients receive,” says Brandy Smuzeski, Clinical Manager with Medical Advantage.
Through these initiatives and timely interventions, elderly patients can avoid medications that are adverse to “What Matters” and costly hospitalization, while medical practices achieve higher care quality and efficiency.
Medical Advantage Helps You Achieve Your Age Friendly Health Systems Improvement Goals
The Medical Advantage mission is, “To simplify the delivery of efficient, high-quality healthcare,” and making healthcare for seniors the best it can be is a fixed part of our endeavor. For decades, our expert consultants have been helping medical practices lower costs and elevate patient care quality from many different angles.
Because your patient care improvement goals are our goals, our experienced consultants specialize in MIPS (Merit-Based Incentive Payment System), ACO, Care Management (including RPM), and Telehealth solutions. What’s more, we help medical practices attract new patients from specific demographics with our practice marketing services, and help to accommodate older patients with ADA website accessibility enhancements.
Get ready for the over-65 population boom and enjoy the benefits of streamlined medical practice operations. Fill out the form below to discuss solutions for the particular needs of your practice with our healthcare management experts.





