Perhaps the best thing about patient engagement is that it is mutually beneficial to both the provider and the patient. Better health outcomes, increased satisfaction with the patient experience, reduction in overall costs, and an enduring provider-patient relationship are all potential gains from patient activation.
Barriers to patient engagement may or may not be obvious, but to optimize your patient experience for better engagement you must be aware of all these obstacles. In this article, we look into several reasons patient engagement is not where it could be – some you may already be familiar with. As you go along, be thinking of possible barriers that limit patient engagement unique to your own patient population.
Why Does Patient Engagement Matter?
Gaps in care (or care management) are a misalignment of patient care from medical best practices. Patient engagement is an effective strategy for resolving preventable and costly poor patient outcomes.
Such gaps can lead to billions of healthcare costs incurred due to:
- Hospital readmissions due to a lack of medication adherence.
- Worsening of health conditions due to avoidance of treatment or not taking medications.
- Partial or total abandonment of a care plan.
Addressing gaps in care is essential for better patient outcomes
What Does Patient Engagement Entail?
Patient engagement is activated when a patient is actively involved and informing decisions for their own wellbeing, along with how the provider accommodates any level of involvement. There are three main areas of patient engagement – decision making, health behavior changes, and chronic disease management.
Assessing Patient Engagement with PAM (Patient Activation Measure)
PAM is a proprietary assessment tool used to determine to what extent a patient population is engaged. It can supply data for research on an organizational level, or it can be used for point of care. It is not part of healthcare regulations, but because it is proprietary, there is a cost to use it.
There are two versions of this 100-point test. The short-term version focuses on 13 measures, while the long-form assessment includes 22 items. This test is used to measure a patient’s ability to:
- Self-manage health problems or illness.
- Take actions that maintain healthy function or reduce a decline in health.
- Be involved in decision making for treatments and diagnostics.
- Cooperate with providers.
- Choose providers decisively based on quality criteria.
- Navigate the healthcare system with ease.
From there, patients are sorted into four activation levels (listed from least to most engaged):
- Unlikely to actively participate in health decisions and expects the doctor to be in charge of it all.
- Gaining confidence and knowledge in their health. Intends to do more for their own health but may not have begun.
- Takes action and considers themselves an equal partner in their healthcare.
- Actively maintains their health and pushes further through Self-advocacy.
Such assessments help healthcare providers find a baseline for an individual patient or their patient population.
Why Is Patient Engagement Important for Your Practice?
The saying goes, “An ounce of prevention is worth a pound of cure.” With the cost of hospitalization being staggeringly high, it is sensible to intervene with preventative care.
Also, some patients do not take their medication or do it properly. This can have severe consequences for patients and is detrimental to patient outcomes. Aside from patients suffering from health decline that could have been avoided, patient outcomes will impact practices tied to the value-based care model.
Why a Patient Engagement Strategy is Key to Success
Anemic patient engagement impacts your quality scoring from CMS (Centers for Medicare & Medicaid Services). To avoid penalties, reap incentives, and reduce administrative burden and stress, patient involvement should be encouraged and supported where feasible.
Clinicians who support patient engagement are a breath of fresh air to those who are discouraged by healthcare experiences. Patient preference for being actively involved in their care decisions, paired with better care outcomes naturally increases the odds of patient loyalty. Some patients will even refer you to family and friends based on their positive experiences.
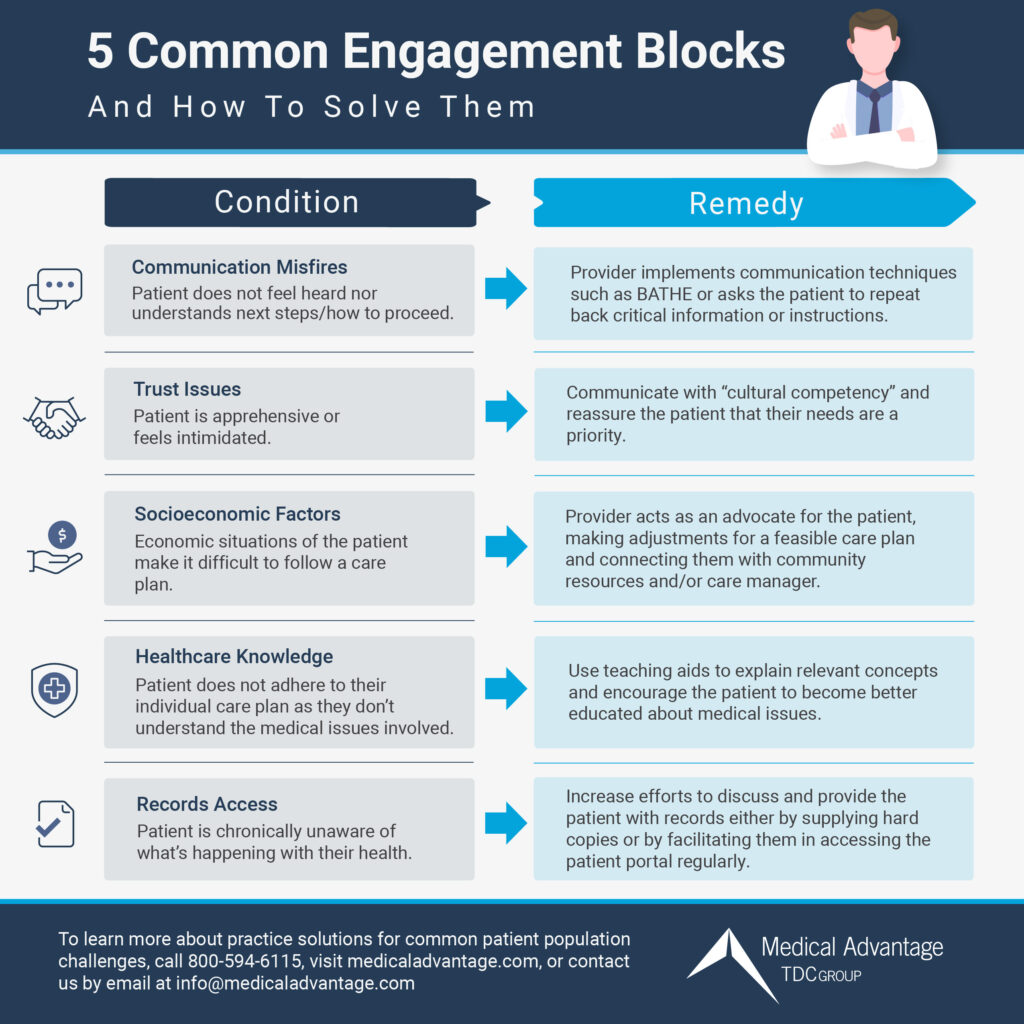
5 Common Barriers to Patient Engagement
Every patient has a unique set of circumstances, so a shortlist like this one will not cover all the possibilities. This list is, however, a starting point for finding barriers to patient engagement that can become improvement opportunities. Levels of patient engagement are:
- Ethical basis – Supports the patient in their autonomy or self-determination.
- Interpersonal basis – Fosters trust in the patient-provider relationship.
- Educational basis – Promotes knowledge, sets reasonable expectations, and mitigates conflict over decision making.
1. Challenges with Communication and Language
Fundamental to any relationship is communication, the patient-provider relationship included. Breakdowns in communication can happen when the patient does not understand what is being thrown at them, or they are too timid to ask clarifying questions. Matters of vital importance can be missed completely in these circumstances.
Of course, a language barrier makes communication quite difficult between a patient and provider. This could be due to nationality or disability. When a patient is not comprehending important information about treatment options, medication, or a care plan, this can have dire consequences.
Potential Solutions for Communication Challenges
The good news is that many patients want to have more meaningful and productive interactions with their providers, but some may be reluctant to engage based on past encounters. To close these gaps, we must look for opportunities to improve communication.
- Make the patient part of the “care team” – Shared-decision making approaches the patient as a partner in their own healthcare. To combat passiveness, assert that the patient is allowed to have self-determination. Body language such as sitting down at the same level can reinforce equality between these roles.
- Ask the right questions – Hone in on what matters to the patient. For example, some use the BATHE approach:
- Background: “What brings you in today?” The complaint is already in the schedule notes, but hearing it directly from the patient gives you the complete story.
- Affect: If the patient has not yet shared how this situation affects them and their quality of life, ask them.
- Trouble: “What worries or bothers you about this?” This will reveal potential barriers to the goals you are trying to reach together.
- Handling: “What have you tried so far?” From here you can recommend those solutions not yet attempted, or help them do the same thing but differently. You might also ask who is available to help in their day-to-day lives.
- Empathy: Acknowledge the difficulty by saying something like, “That must be frustrating for you.”
- Prompt a response – The teach-back method can zero in on what has been missed. You simply ask the patient to repeat back the information back to you so you can hear and correct where things have been missed.
- Verbal and written – Because of differing learning styles, some need to see the information as well as read it. Take-home papers, visual aids, and a summary of the visit accessed through the portal can reinforce what you say verbally.
- Tailor the language – When using medical terms, be sure to interpret these into plain and unsophisticated language.
- Interpretation services and follow-up – For those who are not fluent in English or have communication impairments, qualified interpreters are needed for all communications. Follow up with these patients to ensure that the interpretations were clear.
- Ask for feedback – Ask every patient for feedback about their encounters with providers and other channels (such as portal communications). The patient is the one who determines if your communication strategies are working or not, so there is no better way to confirm this than by asking them directly.
2. Little To No Trust Has Been Established
Experiences that lead to a negative perception of healthcare will cast a shadow over the patient-doctor relationship and generate barriers to patient engagement. Minorities tend to have a broad distrust of the medical field. Unfortunately, this can lead to patients waiting until a condition becomes severe before seeking treatment.
Until a provider earns a patient’s trust, fear and apprehension will get in the way of the best possible care outcomes. One notable impact of these misgivings is the patient withholding significant information for these reasons:
- Feelings of intimidation
- Doubts that they will be heard.
- Feeling that the inquiries are intrusive.
- Skepticism or cynicism toward the medical field and healthcare in general.
- Existing physical or psychological trauma.
Potential Solutions for Nurturing Trust
Developing an empathetic and disarming communication style takes skill that comes from practice. With experience, we learn how to “meet them where they are” and pick up on cues (such as body language). Following through with what you say you will do also goes a long way to establishing trust with hesitant patients.
Sensitivity to a patient’s circumstances is also crucial to building rapport. Cultural competency is, “the ability of systems to provide care to patients with diverse values, beliefs, and behaviors, including the tailoring of health care delivery to meet patients’ social, cultural and linguistic needs.”
Raising awareness of biases can combat alienating interactions. Cultural responsiveness means yielding some power in the patient’s direction, so they feel can feel they have regained some of the control denied to them in the past.
Also be aware of certain language that would be offensive to a patient such as fat-shaming, dismissive of sexuality, ableist, etc.
Cultural competency is,” is “the ability of systems to provide care to patients with diverse values, beliefs and behaviors, including the tailoring of health care delivery to meet patients’ social, cultural and linguistic needs.”
3. Impact of the Patient’s Economic Situation
The economic circumstances of a patient can be a constant barrier without a provider’s assistance. Influential social factors are defined as, “conditions in the environments in which people are born, live, learn, work, play, worship, and age that affect a wide range of health, functioning, and quality-of-life outcomes and risks.” For example, food deserts or religious beliefs impact dietary options, or someone in a remote area may not have access to lab facilities, exercise amenities, or the internet.
Potential Solutions for Advancing Health Equity
To address each aspect of a patient’s economic circumstances, they must first be all accounted for. An SDOH (social determinants of health) screening helps generate a viable customized care plan. Such plans may include:
- Healthy food items that are available and affordable.
- Connecting the patient with social programs that can help with housing, utilities, and food provisions.
- Coordinating transportation to medical appointments or assistance with telehealth options.
- Offering solutions to social isolation and patient safety concerns.
- Being sure that your entire practice is accessible for people with disabilities and impairments, even digitally by making your website ADA-accessible.
- Connecting the patient with a care manager who can oversee that their social determinants are addressed continually.
What these care plans will look like depends on the demographics you serve. Talking with patients and studying the demographic data for your particular population will help you understand common disparities as to what to watch out for when conducting patient intakes.
4. A Lack of Health Literacy and Patient Education
A patient who does not understand a care plan will find it difficult for them to follow. A patient with low health literacy who relies on the provider to do all of the thinking for them is not “activated.” While patients who do a lot of reading online can encounter misinformation that can lead to contentious conversations, the upside of this is the opportunity to have a dialogue that leads to better health literacy.
Potential Solutions for Knowledge Gaps
A patient who educates themselves about health matters is highly engaged in their healthcare. Information handouts are helpful but may not be read if the literature is hard to understand, or the patient does not think it is important. Patient education techniques to consider trying are:
- Coaching-style interactions.
- Video content about specific conditions.
- Pop quizzes to reinforce the most important information.
- Reader-friendly materials that those of all educational levels can understand.
- Use visual aids.
- “Show and tell” – be interactive with the visual aids or take-home materials to point out and explain the parts pertinent to the patient.
- Involve relatives and caregivers.
- Review educational materials periodically to see if any need to be replaced or updated.
- Use your medical website as a digital front door information hub with an on-demand patient education library.
5. Patient Lacks Access to Data and Records
In the past, patient health information was tucked away in a filing system most of the time. These days you can access health records through a portal or track health metrics via personal equipment such as RPMs (remote patient monitoring devices). Readily providing and tracking patient data and records to keep patients aware of where they stand encourages patients to take ownership of their treatment plan.
Potential Solutions for PHI (Patient Health Information) Access
Some commonsense solutions are simply providing the records that will help the patient keep track of their care plan and observe progress as they reach their care plan goals. In addition to ensuring that your EHR and OpenNotes systems are streamlined to deliver patient records, you should also consider:
- Making sure patients know how to access their information via the patient portal by giving in-office or video call tutorials.
- Generating emails that notify a patient when they have a new message from the provider. This message can include reminders to retrieve records.
- Offering print-out copies of records pertaining to their care plan and health goals, especially for those who do not have access to the internet or a home computer.
Medical Advantage Helps Providers Overcome Engagement Gaps
The key to engaging patients is personalized care, but this comes with such a wide spectrum of economic situations and education levels to grapple with. It can be challenging to come up with a cohesive plan to tackle barriers to patient engagement for your whole patient population. A solid medical practice marketing foundation can help improve engagement with your patients as well.
After 20 years in the healthcare space, Medical Advantage has helped providers and administrators of all specialties and organizational levels find effective solutions for modern healthcare challenges, including low patient engagement. Our consultants work at the point of care to streamline your operations, cut costs, and provide the best care possible. Contact us to learn more about our healthcare and IT solutions.



