Considering that physicians spend as much as 50% of the day on documentation, it is important that they have an efficient electronic health record (EHR) that is properly configured for their practice. However, EHR software that was once sufficient can become outdated and unable to meet the needs of modern medical practices.
EHRs have evolved over the years to offer improved customization and interoperability. However, when practices make the move from an old EHR to a new system, they often face the daunting challenge of a major data migration project that introduces the risk of losing critical patient data.
Healthcare providers spend 1–2 hours of extra work each day, including before and after clinic completing “between visit” work – Taming the EHR Playbook | AMA (ama-assn.org)
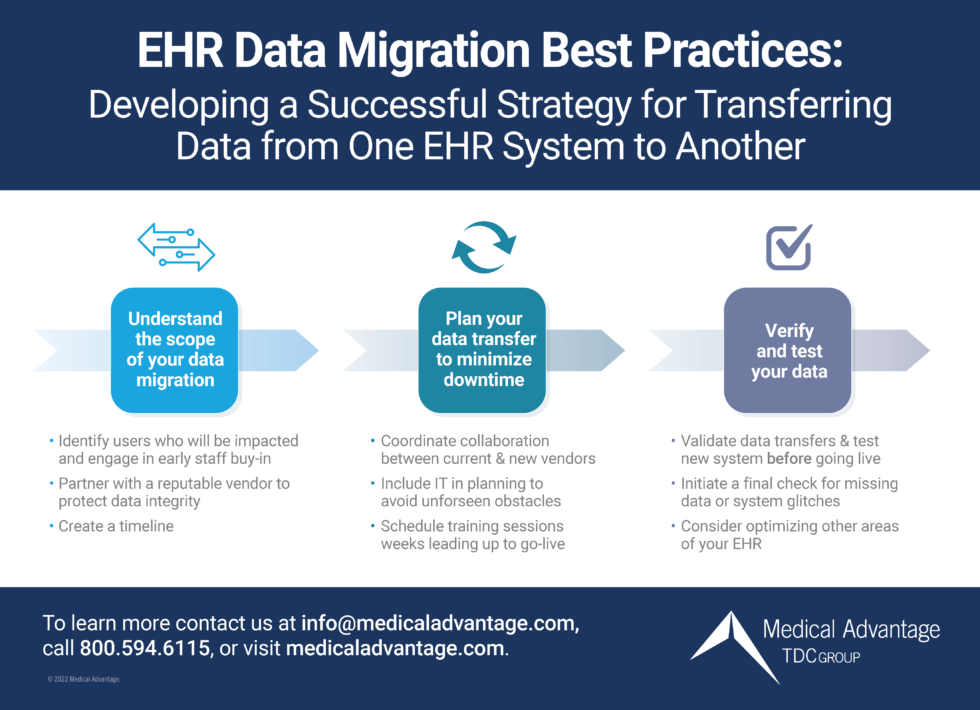
EHR Data Migration Best Practices
EHR migration is the process of transferring data from one EHR system to another. Common reasons for embarking on a new EHR implementation include:
- Lack of integration with other systems
- Poor vendor support and hidden fees
- Unreliable software and constant technical issues
- Lack of mobile access
- Inability of the EHR to scale to your practice goals
Any of these problems, or a combination of them, can add up to a detrimental impact on the quality of patient care.
Understand the Scope of Your Data Migration
Assessing the scope of data migration can be a complex process, especially since every EHR implementation has its own unique nuances. To ensure its success, EHR data migration requires a collaborative team approach. That is why it is important to identify users who will be impacted by the migration and include them when you analyze your data. Questions to ask include:
- What data is essential to convert?
- What additional data would bring value to convert?
- What data can be archived?
- What data may be scanned in and will that be done in-house, via the migration, or by a third party?
After you have established the scope of your EHR data migration, you can begin to map out your plan.
Plan Your Data Transfer to Minimize Downtime
Start by coordinating collaboration between current and new vendors. They should work together to share technical specifications and system requirements to ensure the migration is as seamless as possible. The new vendor’s information technology (IT) staff should be involved in planning the data transfer and available for guidance throughout the process. Both vendors also should help you prepare a timeline for each step of data management and migration.
Understanding and planning for data mapping is critical for minimizing downtime. Working together with the new EHR vendor on a migration solution will help you anticipate potential data mapping issues and troubleshoot them in advance. Also, confirm with both your old and new vendors that they will use the continuity of care documentation (CCD). This is important because these summaries include data about current and past health status that can be shared with other EHR systems if a patient relocates, changes doctors or needs to see a specialist.
Always make sure EHR data is backed up according to HIPAA standards in case unforeseen problems arise during migration. Existing vendors also may be able to help minimize downtime and troubleshoot any issues by providing a testing environment before data migration.
Along with protecting data, minimizing downtime is an important goal throughout the EHR data migration process. If you plan ahead and complete as much work in advance as possible, you can save valuable time and avoid issues post-go-live.
Internally, encourage staff buy-in by emphasizing the importance of migration and how it will ultimately benefit them and their patients. Ask about concerns, such as obstacles to performing job functions during the EHR data migration process.
Be sure that workflows are configured to account for data migration and identify potential issues or errors that may occur and plan how to resolve them. Schedule weekly training sessions for users in the weeks leading up to the go-live date to help them feel confident and acclimate to the new system. Be sure to limit training to only the functionality that is pertinent to each user’s role.
Verify and Test Your Data
Before going live with a new EHR, healthcare facilities must validate that the data transfers are complete and test the new system to ensure it is working properly. After validation, the EHR vendor will do a final check for missing data or system glitches. These steps are critical to avoid obstacles down the road due to missing or incomplete data.
Summary: EHR Data Migration Best Practices
Regardless of the reasons for making the change, protecting data integrity is critical to a successful EHR migration and an inherent responsibility. That is why it is important to partner with reputable EHR vendors and plan carefully well in advance of the target migration go-live date. Staff buy-in also is an essential component of success, so engage your team early in the decision-making process.
Medical Advantage Can Help
When considering purchasing a new EHR, don’t leave optimization off the table. Our expert EHR consultants may be able to help you save time – and money – by finding ways to streamline existing workflows and make your EHR work for you.
However, if you have run out of options for your existing EHR and your staff lacks the time or resources to oversee data migration, we can help make the exchange seamless. That way, you and your staff can focus on what is most important – patient care. Count on us every step of the way for:
- Go-live support with personalized implementation guidance to suit the needs of your practice
- Training and best practices to optimize workflows and leverage new tools along with ongoing technical support
- EHR Helpdesk support with on-demand Q&A and “how-to” advice for simple help requests
Our consultants have years of experience in healthcare and providing EHR support. To begin a smooth and successful data migration process, complete the form below.






