In healthcare, there are many moving parts, plus the many professionals who deliver care, whether seen or unseen by the patients. The more humans can work effectively with machines, the more care will be delivered efficiently, easily, and in a timely manner. Patients have come to expect delays and snags in their healthcare, but through technological improvements, healthcare is countering these biases along the way.
To make the right decisions in healthcare, you must have complete and correct information at the right time. EHR interoperability is the standard that better informs the everyday decisions of medical professionals, as it provides critical data at the moment it is needed. Healthcare providers significantly enhance the delivery of healthcare with the combination of an optimized EHR, efficient workflows, and interoperability.
Understanding EHR Interoperability – What is EHR Interoperability?
For decades, information was siloed across the healthcare system, and it could take weeks for health records to be sent and then processed between entities. The federal government has been pushing for EHR use and interoperability for some time now with policies enacted by such legislation as the HITECH and the Cures Acts. Interoperability in healthcare streamlines the exchange of information for improved community integration, applications integration, public health reporting, as well as improved standards and regulations.
EHR systems allow multiple entities in healthcare to share information with one another. Such entities are primary care providers, specialists, hospitals, long-term care centers, pharmacies, laboratories, and governmental health departments. Interoperability is how we ensure that EHR as a concept works as it should – that information securely gets where it needs to go and is immediately ready to use by whomever it reaches. Like an EMR (electronic medical record), an EHR (electronic health record) is the health record in digital format maintained over the patient lifecycle that includes data such as (but not limited to):
- Demographics
- Progress notes
- Complaints/problems
- Medications
- Vitals
- Immunizations
- Lab results
- Radiology reports
Having complete EHR data readily available allows providers to facilitate care-related measures either directly or indirectly to make evidence-based decisions, manage quality, and report outcomes.
HealthIT.gov defines interoperability as, “Health information technology that— (A) enables the secure exchange of electronic health information with, and use of electronic health information from, other health information technology without special effort on the part of the user; (B) allows for complete access, exchange, and use of all electronically accessible health information for authorized use under applicable State or Federal law; and (C) does not constitute information blocking.”
This official definition outlines the expectations of interoperability. Electronic health information should be exchanged securely, in the most accessible way, without special effort, and to mitigate information blocking. In short, the federal government has made it clear that access and exchange of healthcare information should not be difficult.
Levels of EHR Interoperability
Interoperability is as complex as it sounds, so this will break it down.
- Foundational – The EHR is set up to send and receive data and said data will be ready to use immediately upon receipt.
- Structural – The data itself does not change in essence or in meaning when passed along. With structured messages, the provider gets unaltered information in a meaningful and sharable format for the database.
- Semantic – The data can be understood between systems. A healthcare entity cannot use data that they cannot read or interpret. Standardized data exchange ensures that everyone receives data in a ready-to-use format.
- Canonical – Patient information extracted from the source systems or inserted into another source system data structure.
- Syntactic – Inserts patient data into the applicable message structure, or extracts patient information from the message structure.
- Physical – Messages transmitted to the target system.
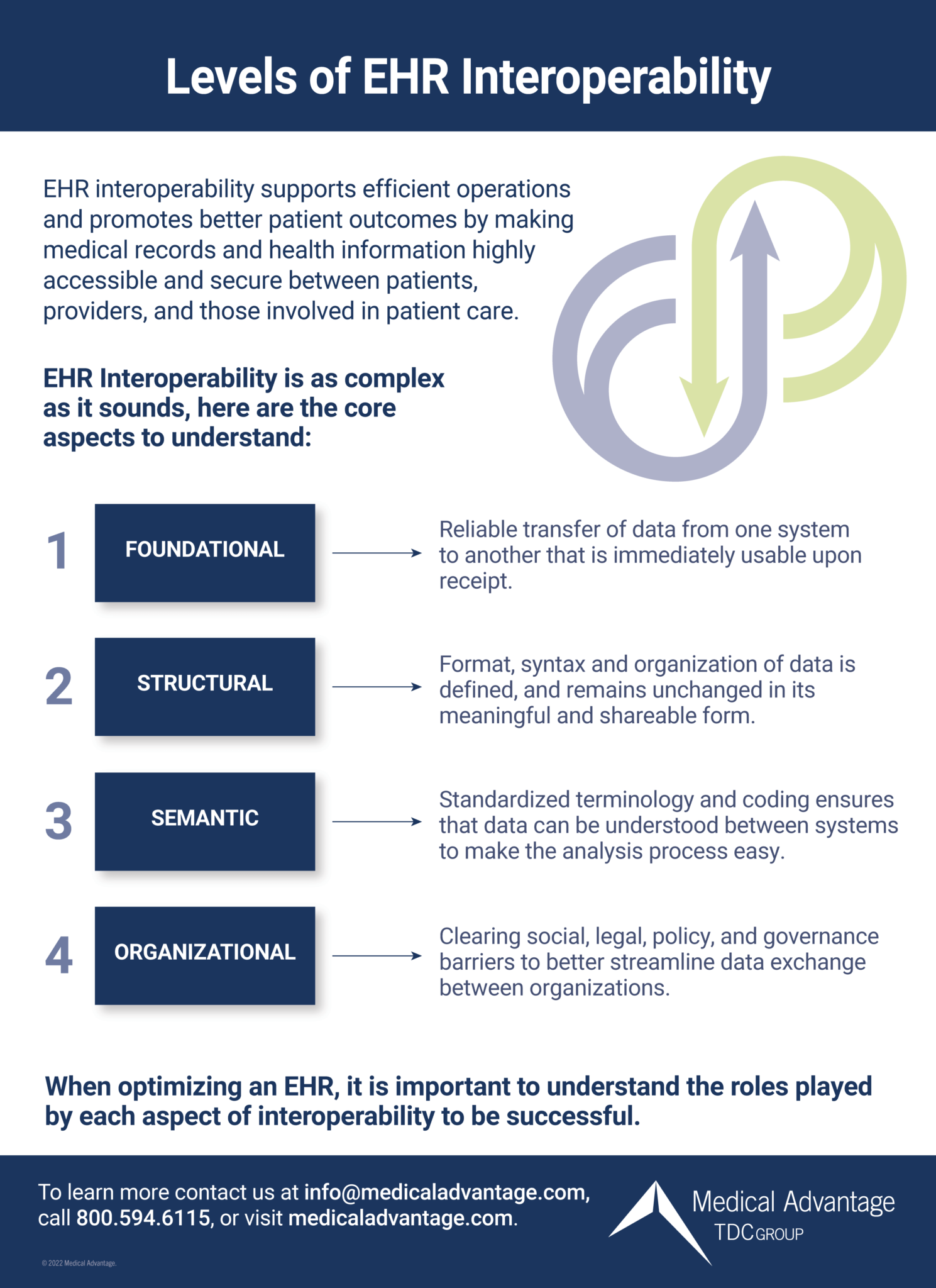
All levels must be engaged and calibrated for EHRs to be successful. Interoperability also considers:
- How well information is both processed and managed
- How well applications interact with users
- How well systems communicate with one another
- The best way for systems and applications to integrate with user devices (such as mobile devices).
Interoperability Standards
EHR interoperability is most successful when everyone involved adheres to the same rules and guidelines. We need standard methods for security, data transport, format, structures, meanings of codes/terms, and the like. Standards are created by SDOs (consensus-based standards committees) to establish set rules that work best for all interoperability interactions.
Standards with staying power have a high adoption rate (and become de facto within the industry), do well to meet the needs of the user base, are inexpensive or open-source, or are government-mandated. Such standards are set to benefit the healthcare community as a whole, level the playing field, and improve the EHR user experience.
A lack of standardization brought on by a myriad of different EHRs in use among entities means we still have progress to make to become a fully interoperable as a healthcare system. Differing interfaces, various coding languages, and inconsistent language terms are why the meaningful sharing of information continues to be a challenge in many areas of healthcare.
MIPS Promoting Interoperability (PI)
Interoperability is such a priority of the government that they have made it part of the MIPS (merit-based incentive payment system) scoring process. MIPS Promoting Interoperability (PI) is a requirement and scoring category and promotes patient engagement by the electronic exchange of information using certified electronic health record technology (CEHRT). This category replaces the Meaningful Use program.
This measure is intended to improve patient access to health information, but it is also geared towards improved information exchange between pharmacies and providers. This standard is also the “systematic collection, analysis, and interpretation of healthcare data.”
Why Is EHR Interoperability Important
Interoperability is measured by how easily medical records and health information transmit from one system or provider to another. It allows EHRs to communicate securely with entities external of a practice such as pharmacists, specialists, and even patients. It allows everyone involved to be well prepared for the next step, whatever that step may be. Additionally, an EHR will not be able to serve its purpose without interoperability – the purpose being that an EHR is set up to share critical data with external entities.
EHR interoperability helps:
- Providers do better – With ready access to critical healthcare data, providers can avoid errors by having all the information they need to make a more informed decision for patient care. This can even help prevent erroneous diagnoses that lead to malpractice lawsuits.
- Patients do better – You have been a patient at some point. What is it like, as a patient, to be told that your records have not arrived on time for your consultation? What if you are told that you will go another day without medication because of a mix up between your provider and the pharmacy? Or told that you have to do the same bloodwork or x-rays that you just did a month ago for another doctor? Interoperability means that information about your care is not only going where it needs to go, but that it gets there quickly and is ready for use immediately so that patients experience less inconvenience.
- The bottom line – Efficiency means that practices can recover hours of wasted time, so they will now have more time to see more patients and expand the patient base. It also means that hours of staff labor will be spent on what improves care rather than wrangling data and records. Also, for practices who look forward to shared savings from CMS quality scoring, EHRs are a mandated part of delivering quality care for CMS patients.
EHR Interoperability Challenges
Though much effort goes into setting standards, EHR design is far from universal, especially when there are so many EHR vendors in hefty competition to offer the most superior product. Common interoperability problems include:
- Not comprehending privacy laws sufficiently, or insecure data transmission.
- Misalignment of payment incentives.
- Standardization gaps, or standardization rules that cannot be enforced.
- Differing EHR designs that may not be equipped to readily adopt interoperability standards.
- Too much data without the resources to digest it.
- Adding on more partners (an acquisition, for example) means a sizeable task of assimilating the health data to a uniform format.
- Workflows that are incompatible with EHR inoperability.
- Not all payers are willing to participate or share valuable data.
- Records not matched to the right patient, or otherwise conflicting information.
- Inability to measure interoperability performance among entities.
EHR interoperability continues to improve within healthcare, and despite the challenges your organization can do its part to make interoperability successful with an optimized EHR.
EHR Interoperability Solutions
Wherever there are delays, missing records, incomplete data, or information that is there but unusable, there are interoperability problems. A fully interoperable EHR is one that both gives and receives patient data promptly, without alteration, and in a format that can be readily used. When handling patient data, it is important to remember that these records belong to a human being (the patient) and not the medical entity.
Here are tips on best practices for EHR interoperability:
- Do a complete assessment or audit of your EHR to create an interoperability improvement plan.
- Support a patient-centered approach to healthcare by making it
sas easy as possible to access records, test results, and make information requests through the patient portal. - Encourage providers and medical staff to use standard medical terminology when documenting patient care so that everyone is on the same page. Adopt standardized code systems and data sets, conformance assessment and certification, and the associated supporting tools.
- Ensure that the identifying information about the patient is accurate and complete to avoid a patient being mistaken for another. Secure connectivity, digital identities, common directories to make accurate connections and identifications.
- Design a workflow that promotes the most efficient interoperability and integrates automation, where appropriate. RPA (robotic process automation), AI (artificial intelligence), and ML (machine learning) can remove unnecessary steps and delays in the movement of data and records.
Optimize Your EHR to Maximize Interoperability
Ensuring that your EHR is interoperable is a challenging and complex undertaking. With the help of seasoned EHR experts, you can address existing interoperability issues, uncover issues not yet known, and resolve obstacles that come from external stakeholders.
EHRs must be interoperable to function as intended, and Medical Advantage is here to ensure that your EHR is most efficient in getting patient data where it needs to go. Those participating in shared savings programs (such as MIPS) benefit from EHR optimization, so they will get credit for all the efforts they put into delivery of high-quality care.
Training support is also provided to ensure that each staff member understands their role in EHR interoperability. Learn more about our proven EHR services and request a no-obligation initial consultation today!






