Providers participating in the Merit-based Incentive Payment System (MIPS) program are hoping for a net positive outcome Performance Year 2023. Whether you are creating a MIPS quality and reporting plan from scratch or just updating one, knowing the core basics of a successful MIPS strategy will best guide the process.
From our years of experience helping value-based care providers maximize reimbursements from CMS, we created a step-by-step guide on how to structure your MIPS game plan. From this template, you can apply proven best practices to plan for your MIPS performance goals.
To view our full overview for changes to expect in 2023, read our article here.
5 Step MIPS Checklist Overview
- Determine Which MIPS Data You Need to Submit
- Determine Which MIPS Framework Your Should Use to Submit Your Data
- Research and Understand Changes to MIPS Scoring for 2023
- Evaluate Your Projected MIPS Performance and Adjust Accordingly
- Hire a MIPS Expert
1. Determine Which MIPS Data You Need to Submit
The first item on our MIPS checklist involves looking at the specific data providers must report. While most providers who have previously participated in MIPS are likely to, by now, be somewhat familiar with the different reporting categories, it bears revisiting what providers are required to report for each MIPS performance year.
Just as there are major program changes each year, there are also smaller, category and measure-specific changes that must be reviewed. Do not make the mistake of assuming that all measures you reported previously are still available in 2023, or that the specifications for those measures have remained static.
Use the QPP Resource Library to dive into those specifications for Quality, Improvement Activities, and Promoting Interoperability to make sure you are completely and accurately reporting your data. This will maximize your chances of scoring well and avoiding potential headaches if you are audited in the future.
2. Determine Which MIPS Framework You Should Use to Submit Your Data
The next step is to determine which framework your organization will use to submit your data to CMS. When MIPS started in 2017, no one would have said the MIPS reporting framework was simple, but at least there was only one option. Now you have several frameworks to choose from.
These frameworks include Traditional MIPS as you have known it all along, APM Performance Pathway (APP) for providers who participate via MIPS APMs, or the MIPS Value Pathways (MVPs) which are designed around specific populations of patients. This expansion of options is a double-edged sword because with increased flexibility comes increased complexity. Success in any framework will be tied to understanding the associated pros and cons specific to your practice circumstances.

3. Research and Understand Changes to MIPS Scoring for 2023
To achieve your full potential in quality scoring, you must become aware of all the scoring changes and how they apply to your particular patient population and practice size. As you grasp the changes for 2023, you can evaluate past MIPS performance against new scoring standards.
The sooner you complete this evaluation, the better. Without preparation, when it is time to report back to CMS, you can easily end up with a score lower than expected. In short, don’t wait until it is too late to make adjust processes and reporting.
4. Evaluate Your Projected MIPS Performance and Adjust Your Strategy
Armed with the insights from your enhanced understanding of the MIPS changes proposed for 2023, it is time to take a critical look at your organization’s performance. Will your organization be able to continue scoring at a high enough level to avoid being penalized? Will your organization have a difficult time adjusting to a more heavily weighted cost category? While such reflections can be both difficult and time-consuming, they are of the utmost importance.
Participating in MIPS is a long game. Changes to EHR documentation, workflows, and strategies take time to implement and even longer to affect changes in your performance rates. Rewards for your efforts to improve your MIPS performance will come at least a year after your MIPS performance data is submitted.
It is crucial that your organization begins optimizing and updating its operational and reporting strategy for MIPS as soon as possible to get ahead of increasingly demanding and competitive MIPS requirements. Choosing to wait can be costly in the future.
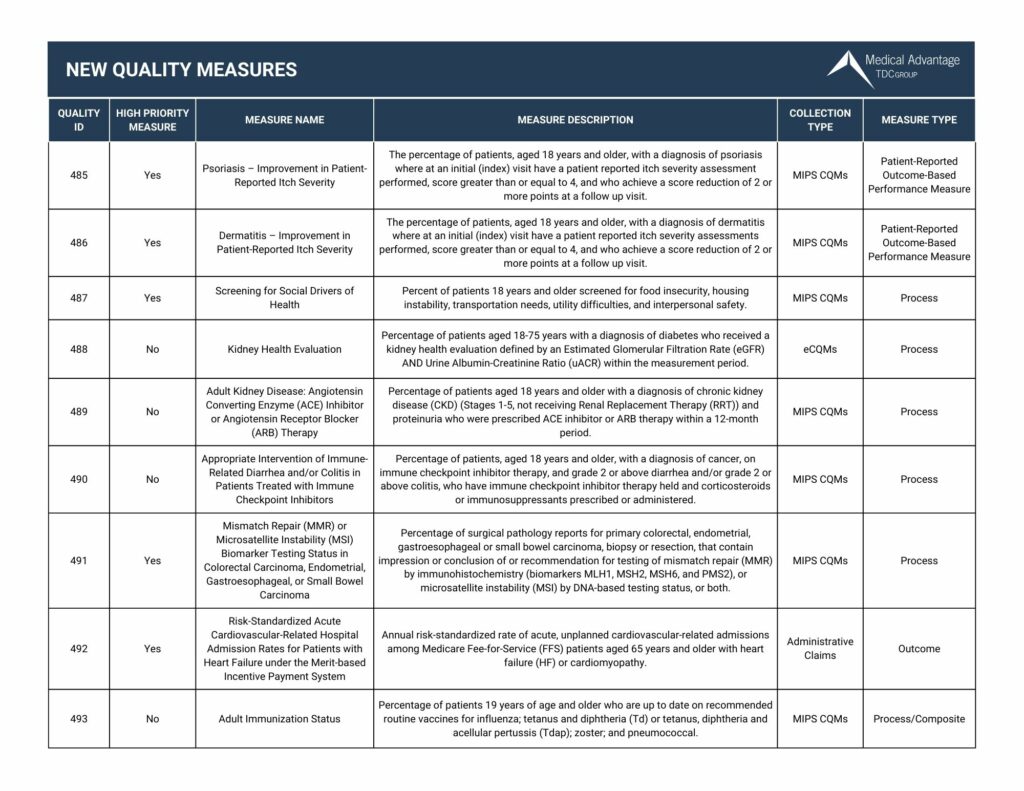
New MIPS Quality Measures for 2023
View our chart below for the new quality measures in 2023. Want to view all the updates for 2023? Click here to download our 2023 Quality Measures Guide
5. Team Up with Consultants with MIPS Expertise
To say that navigating CMS programs like MIPS is challenging is an understatement. “When I was managing my own practice, I spent so much time after hours reading MIPS rules,” says Beth Hickerson, MIPS expert and Medical Advantage’s Senior Consultant for Quality and Healthcare Transformation. “Just understanding MIPS is a full-time job.”
For providers and staff already busy with running a practice and caring for patients, taking time to understand this complex and mammoth piece of healthcare legislation can be daunting. But expert MIPS consultants who understand MACRA and industry best practices are here for you. Medical Advantage’s experienced team can guide you through the MIPS process to maximize reimbursement opportunities and avoid penalties, leading to a more efficient and profitable practice.
To find out more about how we can help, contact our MIPS consulting team today.





